‘Physiotherapy is a science based profession and takes a whole person approach’ (The Chartered Society of Physiotherapy 2024)
With this in mind, part of the physiotherapists’ role is to holistically assess and treat patients. It is important to note physiotherapists are not nutritionists and if you need nutritional help then they are the most qualified people to do so. However, I think physiotherapists should have an awareness of nutritional benefits with their patients, especially after a soft tissue or bony injury.
Whether it’s human, horse or hound we all have something called an energy reserve. This is like a treasure box filled with available energy for the body to use. When there is an injury the demand for energy increases because the body needs to try and repair, so instead of getting a larger treasure box we need to fill the space the current one has to offer.
‘We need to optimise the body’
If our available energy is low rehabilitation will be affected because it’s harder to meet the demands e.g. an exercise programme. This does not mean however for example following surgery and in post operative recovery, you can eat or feed your dog an unlimited amount of food. If you do this energy can be stored as fat and then you have a whole other dilemma on your hands. It is all about balance and awareness of what the body needs.
There are 3 main macronutrients we need to optimise the body following injury;
Fibre aids with managing diabetes and supports the microbiome – we have all heard the saying ‘the gut is the second brain’. If we have a happy microbiome we have a happier body.
Protein has a role with haemoglobin (red blood cells which bind oxygen in the blood). Increasing blood flow to an injury site is one key aim when physiotherapist’s treat an injury, whether that is massage, laser, heat etc. Blood flow will improve healing so we need haemoglobin and adequate protein intake to help us. Protein is also the building blocks for tendons (amino acids) and muscle, alongside the immune system and bone health.
Dietary Fats are really important for cell membrane lining, brain development and maintenance. Fats help line our nervous system (something called myelin) which is the transport network for nerves around the body and brain. Insufficient dietary acids in our food can affect the absorption of certain vitamins also such as A,D,E & K. So we need fats in our diet but we’re looking for the ‘healthy ones’ which are unsaturated. Below display some ideas.
| Dietary Fats (Omega 3, 7 + 9 = unsaturated Fats) | ||
| Omega – 3 | Omega 7 + 9 | Saturated Fat |
| Salmon | Olives | Red Meat + Pork |
| Tuna/Cod/Shrimp | Avocados | Butter/cream/cheese |
| Mackeral | Sesame Seeds | Poultry Skin |
| Fish Oils | Peanuts | Coconut Oil |
| Flaxseeds | Cashews | Palm Oil |
| Chia Seeds | Hazelnut | Cocoa Butter |
| Soybeans | Sunflower/Sesame Oil | Animal Fats |
So what does all this mean?
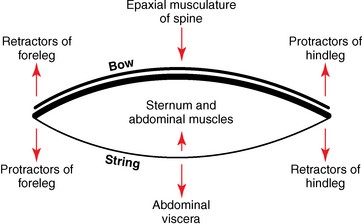
Here is a graphic by Physio Network detailing what happens when there is a soft tissue injury.
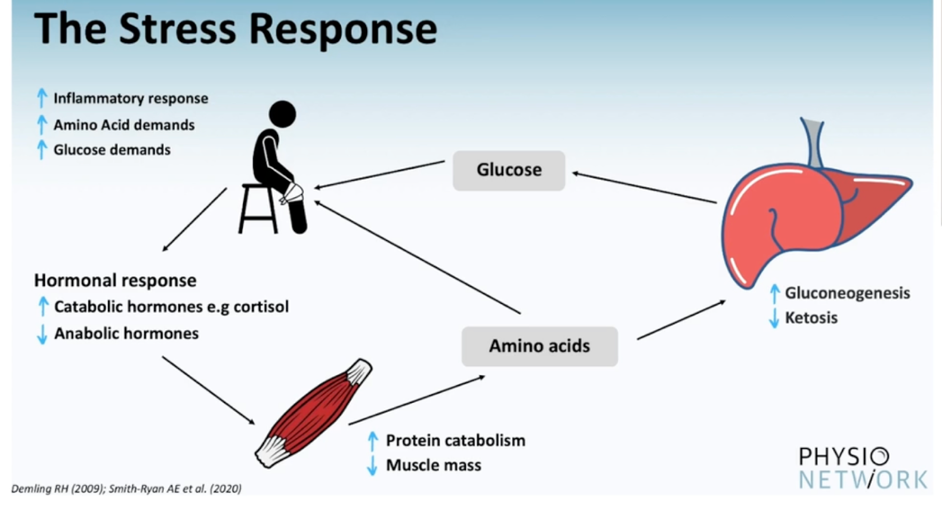
- The animal or human injures themselves and is diagnosed or suspected to have sustained a soft tissue injury. There is an immediate inflammatory response (swelling/bruising) and it is at this point we need protein to help build and repair the injured muscle.
- Hormones come to the rescue to break down (catabolic reaction) other sources of amino acids. To get these amino acids (some is stored in muscle) muscle mass is reduced from other areas.
- The liver undergoes gluconeogenesis which means it increases energy to meet the demands of the soft tissue injury and help healing.
The idea of nutrition in a soft tissue injury is to stack the odds against the injury so you optimise the body for healing. Now animals and humans can heal with sub optimal nutrition, sub optimal sleep and high stress levels but why would you not help the injury as much as possible?
The question which rises here is, do you adapt yours or your animals diet when you/they have a soft tissue or bony injury?
If you want to know more about how much intake you need on a daily basis these links can be useful;
https://www.who.int/news-room/fact-sheets/detail/healthy-diet